Facetogenic Lower Back Pain: Uncovering a Common Cause of Discomfort
Lower back pain is a widespread issue that affects millions, and for some, the source of their discomfort lies in the facet joints of the spine. Facetogenic lower back pain, caused by dysfunction or degeneration in these small but critical joints, can make everyday activities like sitting, standing, or twisting painful.
Understanding this condition is essential for finding targeted relief and improving quality of life. In this blog post, we’ll explore what facetogenic lower back pain is, its causes, symptoms, and treatment options, all explained clearly for a general audience.
What is Facetogenic Lower Back Pain?
Facet joints, also called zygapophyseal joints, are small, paired joints located at the back of each vertebra in the spine, including the lumbar spine (lower back, L1-L5). These joints connect the vertebrae, allowing movement like bending and twisting while providing stability. Each facet joint is lined with cartilage and surrounded by a capsule, with nerves that transmit pain signals when irritated.
Facetogenic pain occurs when these joints become inflamed, damaged, or degenerated, leading to localized or radiating discomfort. Unlike disc-related pain or sciatica, facetogenic pain is typically centered in the lower back and does not usually radiate far into the legs. It’s estimated to account for 15-45% of chronic lower back pain cases, per a 2020 study in Pain Physician, making it a significant but often underdiagnosed condition.
Causes of Facetogenic Lower Back Pain
Facetogenic pain results from irritation or damage to the facet joints, triggered by various factors:
- Degenerative Arthritis: Osteoarthritis causes cartilage wear in the facet joints, leading to bone-on-bone friction, inflammation, or bone spurs (osteophytes).
- Trauma or Injury: Whiplash, falls, or heavy lifting can strain or injure the facet joints or their capsules.
- Repetitive Stress: Prolonged sitting, poor posture, or repetitive bending/twisting (e.g., in sports or manual labor) can overload the joints.
- Synovial Cysts: Fluid-filled sacs in the facet joint can form, compressing nearby nerves.
- Spinal Conditions: Spondylolisthesis (vertebra slippage) or scoliosis can stress facet joints, causing pain.
- Post-Surgical Changes: Lumbar fusion surgery can increase stress on adjacent facet joints, leading to degeneration.
Risk factors include aging (facet degeneration increases after age 40), obesity, sedentary lifestyles, or occupations involving repetitive spinal movements.
Symptoms of Facetogenic Lower Back Pain
Facetogenic pain has distinct characteristics that set it apart from other back pain conditions:
- Localized Lower Back Pain: Aching, burning, or sharp pain in the lower back, often on one or both sides of the spine.
- Pain with Movement: Worsened by bending backward, twisting, or standing for long periods, as these stress the facet joints.
- Relief with Position Changes: Pain often eases when lying down, sitting, or bending forward, which reduces joint pressure.
- Stiffness: Limited flexibility in the lower back, especially in the morning or after inactivity.
- Radiating Pain: Discomfort may spread to the buttocks, hips, or upper thighs, but rarely below the knee (unlike sciatica).
- Tenderness: Pressing on the facet joints (along the spine) may provoke pain.
Symptoms may fluctuate, worsening with activity or stress, and can be mistaken for discogenic pain or sacroiliac dysfunction.
Diagnosing Facetogenic Lower Back Pain
Diagnosing facetogenic pain is challenging due to its overlap with other conditions (e.g., disc herniation, sacroiliac joint pain). A thorough evaluation includes:
- Medical History: Discussing pain onset, location, triggers (e.g., bending backward vs. forward), and history of trauma or arthritis.
- Physical Exam: Testing range of motion, palpating the spine for tenderness, and assessing movements that provoke facet joint pain (e.g., extension or rotation).
- Imaging:
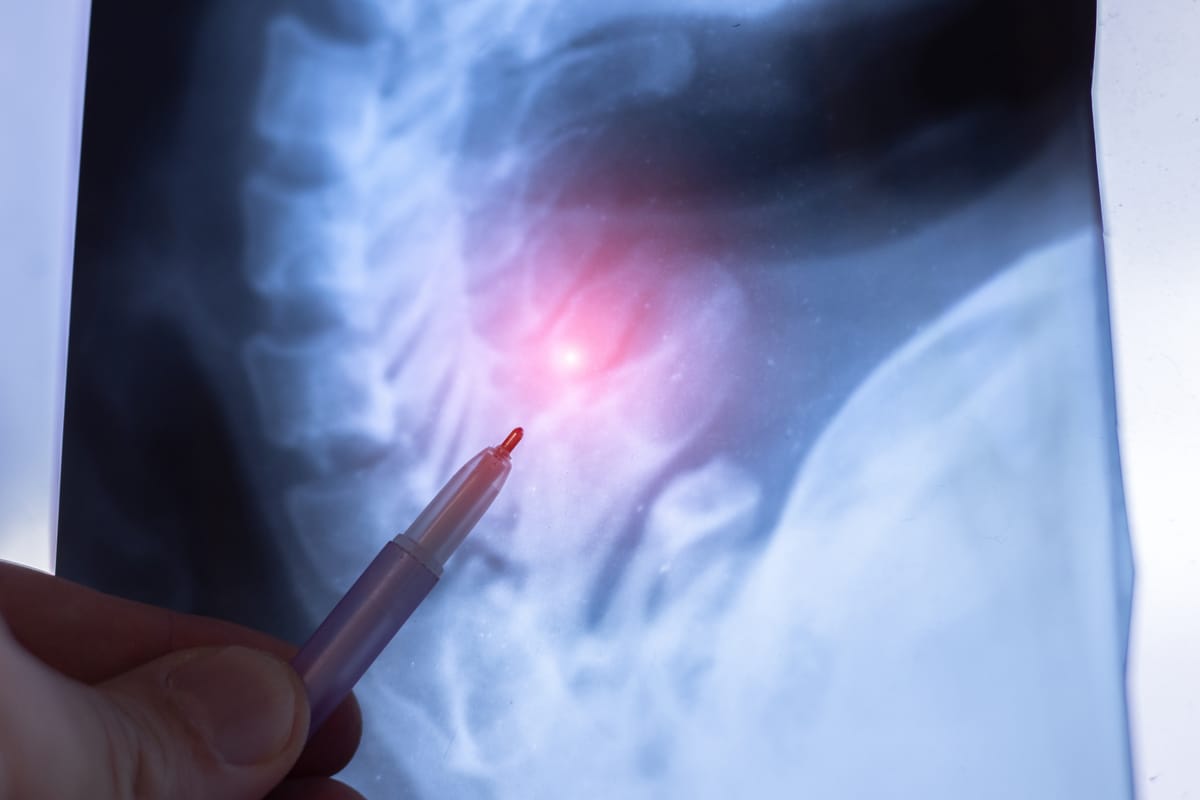
- X-rays: To detect arthritis, bone spurs, or alignment issues.
- MRI or CT: To visualize joint degeneration, synovial cysts, or rule out disc or nerve issues.
- Diagnostic Injections: Fluoroscopy- or ultrasound-guided medial branch blocks (anesthetic injections near the nerves supplying the facet joints). Pain relief confirms the facet joints as the pain source.
A 2021 study in Pain Medicine found that combining physical exams with diagnostic injections improves diagnostic accuracy for facetogenic pain by 85-90%.
Treatment Options for Facetogenic Lower Back Pain
Treatment aims to reduce inflammation, relieve pain, and improve function, starting with conservative approaches and escalating as needed.
- Conservative Treatments
- Physical Therapy: Strengthening core and back muscles, improving posture, and using exercises to reduce facet joint stress. Flexion-based stretches (e.g., bending forward) often help.
- Medications:
- NSAIDs (e.g., ibuprofen) for inflammation and pain.
- Muscle Relaxants for spasms.
- Neuropathic Drugs (e.g., gabapentin) for nerve-related pain.
- Lifestyle Changes: Weight loss, ergonomic adjustments (e.g., proper seating), and avoiding activities that worsen pain (e.g., repetitive bending backward).
- Activity Modification: Short-term rest followed by gradual return to activity to prevent deconditioning.
2. Interventional Procedures
- Facet Joint Injections: Fluoroscopy- or ultrasound-guided corticosteroid and anesthetic injections into the facet joint to reduce inflammation. A 2020 study in Pain Physician found 60-70% of patients had relief for 1-3 months.
- Medial Branch Radiofrequency Ablation (RFA): Uses heat to disrupt pain-transmitting nerves (medial branches) supplying the facet joints, offering relief for 6-12 months, per a 2019 study in Journal of Pain Research.
- Intra-articular Injections: Less common, targeting the joint capsule directly.
- Endoscopic Facet Rhizotomy: Obliterates the nerve through a tiny incision, for more durable pain relief without a large surgery.
- Minimally Invasive Facet Fusion: Much less invasive than traditional surgery, resulting in effective stabilization of the spine.
3. Surgical Treatments
- Spinal Fusion: For severe, persistent facet joint pain with instability or spondylolisthesis, fusing vertebrae to stabilize the spine. A 2021 study in The Spine Journal reported 60-70% pain relief at 1 year, though it’s rarely needed (5-10% of cases).
- Surgery is a last resort after conservative and interventional treatments fail.
4. Complementary Therapies
- Chiropractic Care: Gentle adjustments to improve spinal alignment, with caution to avoid overstressing the joints.
- Acupuncture: May reduce pain perception, with some studies showing benefits for chronic back pain.
- Psychological Support: Cognitive-behavioral therapy or mindfulness to manage chronic pain’s emotional toll.
A 2021 review in Global Spine Journal found that 60-70% of facetogenic pain patients improve with conservative treatments within 3-6 months, with interventional procedures helping those with persistent symptoms.
Living with Facetogenic Lower Back Pain
Facetogenic pain can feel limiting, affecting work, hobbies, or sleep. Keep a pain diary to track symptoms and triggers, and share details with your healthcare team to guide treatment. Support groups, through organizations like Spine-Health (spine-health.com) or the North American Spine Society (spine.org), or online platforms like Reddit, offer a space to connect with others and share coping strategies.
Emotional support is vital, as chronic pain can lead to stress or depression. Lean on counselors, family, or friends for encouragement. Practical steps, like using a lumbar support cushion, alternating positions, or practicing gentle stretches, can help manage symptoms.
Why Awareness Matters
Facetogenic pain accounts for a significant portion of chronic lower back pain, yet it’s often misdiagnosed as discogenic pain, sacroiliac dysfunction, or muscle strain, per a 2020 study in Osteoarthritis and Cartilage. Raising awareness ensures patients receive accurate diagnoses and targeted treatments, preventing prolonged suffering.
If you’re experiencing chronic lower back pain, especially worsened by bending backward or twisting, consult a spine specialist to explore whether facetogenic pain is the cause. Resources like Spine-Health or the American Academy of Orthopaedic Surgeons (aaos.org) offer valuable information and support.
By understanding facetogenic lower back pain, we can empower those affected to seek relief and reclaim their mobility. Let’s keep the conversation going—no one should face this pain alone.
Disclaimer: This blog post is for informational purposes only and not a substitute for professional medical advice. Consult a healthcare provider for diagnosis and treatment of facetogenic lower back pain.



