Insufficiency Fractures Due to Osteoporosis: Understanding the Risks and Finding Solutions
Osteoporosis is a silent condition that weakens bones, making them fragile and prone to breaking under minimal stress. One of the most serious consequences of osteoporosis is insufficiency fractures, which occur when weakened bones crack under normal daily activities, like walking or lifting light objects. These fractures can cause significant pain, disability, and reduced quality of life, especially in older adults. Understanding insufficiency fractures and their connection to osteoporosis is crucial for prevention and management. In this blog post, we’ll explore what insufficiency fractures are, their causes, symptoms, diagnosis, and treatment options, all explained clearly for a general audience.
What Are Insufficiency Fractures and Osteoporosis?
- Osteoporosis: A condition where bones lose density and strength, becoming porous and brittle due to reduced bone mass. It affects about 10% of adults over 50 globally, with women at higher risk, per a 2020 study in Journal of Bone and Mineral Research.
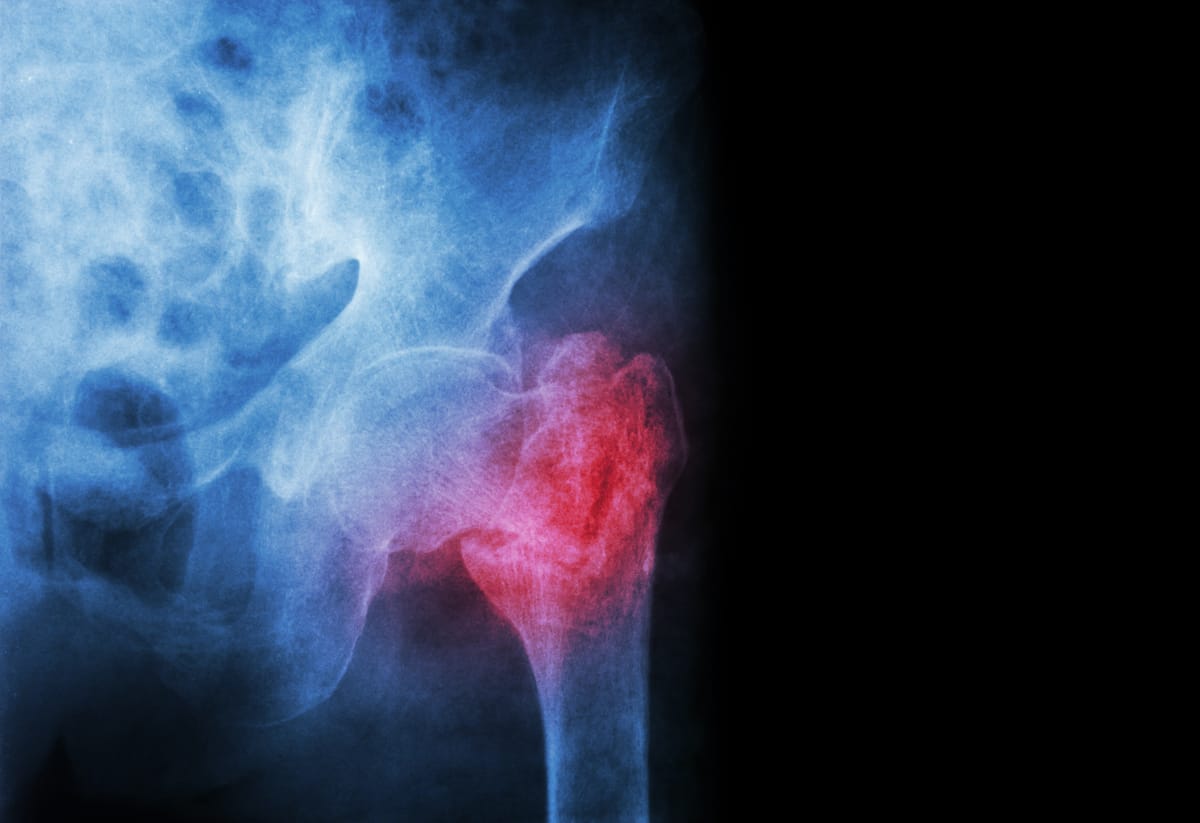
- Insufficiency Fractures: Fractures that occur in weakened bones under normal or minimal stress, without significant trauma (unlike traumatic fractures from falls or accidents). These fractures are a hallmark of osteoporosis and typically affect the spine, hips, pelvis, or wrists.
Insufficiency fractures happen because osteoporotic bones lack the strength to withstand routine forces, leading to cracks or breaks. They are a major cause of disability, with vertebral and hip fractures being the most common, affecting 20-30% of osteoporosis patients, per a 2021 study in Osteoporosis International.
Causes of Insufficiency Fractures in Osteoporosis
Insufficiency fractures result from the interplay of weakened bones and everyday stresses. Key factors include:
- Bone Loss in Osteoporosis: Reduced bone mineral density (BMD) and poor bone quality make bones fragile. This is driven by:
- Aging: Bone density peaks in your 20s and declines after age 50, especially in postmenopausal women due to estrogen loss.
- Hormonal Changes: Low estrogen or testosterone reduces bone formation.
- Medical Conditions: Rheumatoid arthritis, hyperthyroidism, or malabsorption disorders (e.g., celiac disease) increase bone loss.
- Medications: Long-term use of corticosteroids, anticonvulsants, or certain cancer treatments weakens bones.
- Minimal Stress or Activity: Everyday actions like bending, lifting, walking, or even coughing can trigger fractures in osteoporotic bones.
- Common Fracture Sites:
- Vertebral Compression Fractures: Collapsing vertebrae in the spine, often from sitting or standing.
- Hip Fractures: Breaking at the femoral neck or pelvis, often from minor movements.
- Pelvic or Sacral Fractures: Cracks in the pelvis or sacrum, common in older adults.
- Wrist or Other Fractures: Breaks from light impact or pressure.
Risk factors for insufficiency fractures include age (over 65), female gender, family history of osteoporosis, low body weight, smoking, excessive alcohol use, and sedentary lifestyles.
Symptoms of Insufficiency Fractures
Insufficiency fractures may go unnoticed initially, especially in the spine, but symptoms often emerge as the condition progresses:
- Sudden or Gradual Pain:
- Spinal Fractures: Sharp or aching back pain, often in the mid or lower back, worsened by movement or standing.
- Hip or Pelvic Fractures: Pain in the hip, groin, or buttocks, worse with walking or weight-bearing.
- Wrist Fractures: Pain or tenderness after minimal impact.
- Reduced Mobility: Difficulty walking, standing, or performing daily tasks due to pain or weakness.
- Height Loss or Stooped Posture: Vertebral fractures can cause a hunched back (kyphosis) or loss of height.
- Deformity: Visible changes, like a curved spine or difficulty standing upright.
- No Clear Trauma: Fractures occur without a significant fall or injury, distinguishing them from traumatic fractures.
Symptoms may be subtle, and some fractures (e.g., vertebral) are detected only after imaging. A 2020 study in The Lancet noted that 50-70% of vertebral fractures are asymptomatic initially, making early diagnosis critical.
Diagnosing Insufficiency Fractures and Osteoporosis
Diagnosing insufficiency fractures and underlying osteoporosis involves a combination of clinical evaluation and testing:
- Medical History: Discussing symptoms (e.g., sudden back pain), fracture history, and risk factors (e.g., menopause, steroid use, or family history).
- Physical Exam: Checking for tenderness, deformity (e.g., kyphosis), or reduced mobility. Tests for balance or gait assess fall risk.
- Imaging:
- X-rays: To detect fractures, vertebral collapse, or bone deformities. Often the first step when a fracture is suspected.
- MRI or CT: To visualize subtle fractures (e.g., sacral or stress fractures) or assess soft tissue/nerve involvement.
- Bone Density Testing (DEXA Scan): Measures bone mineral density (BMD) with a T-score:
- Osteopenia: T-score between -1.0 and -2.5.
- Osteoporosis: T-score -2.5 or lower.
- Severe Osteoporosis: T-score -2.5 or lower with fractures.
- Blood and Urine Tests: To rule out secondary causes of bone loss, such as:
- Calcium or vitamin D levels.
- Thyroid or parathyroid function.
- Bone turnover markers (e.g., C-telopeptide).
- FRAX Tool: Estimates 10-year fracture risk based on BMD, age, and other factors to guide treatment.
A 2021 study in Osteoporosis International found that DEXA scans combined with X-rays accurately diagnose osteoporosis and insufficiency fractures in 90-95% of cases.
Treatment Options for Insufficiency Fractures and Osteoporosis
Treatment focuses on managing fractures, relieving pain, and addressing underlying osteoporosis to prevent future fractures. A multidisciplinary approach is key.
1. Managing Insufficiency Fractures
- Pain Relief:
- Medications: NSAIDs (e.g., ibuprofen), acetaminophen, or short-term opioids for severe pain.
- Bracing: A back brace for vertebral fractures to support the spine and reduce pain during healing.
- Rest and Activity Modification: Limited activity for 4-8 weeks to allow fracture healing, followed by gradual return to movement.
- Interventional Procedures:
- Vertebroplasty or Kyphoplasty: Minimally invasive procedures injecting bone cement into fractured vertebrae to stabilize them and relieve pain. A 2020 study in Pain Physician found 70-80% pain relief in vertebral fracture patients.
- Surgery: For severe hip or pelvic fractures, procedures like hip replacement or internal fixation may be needed (rare for insufficiency fractures).
- Physical Therapy: Gentle exercises to restore mobility and strength after initial healing, focusing on balance to prevent falls.
2. Treating Osteoporosis
- Medications:
- Bisphosphonates (e.g., alendronate): Slow bone loss and reduce fracture risk by 30-50%, per a 2020 study in Journal of Bone and Mineral Research.
- Parathyroid Analogues (e.g., teriparatide): Stimulate bone formation, ideal for severe cases.
- Denosumab: Inhibits bone resorption, reducing fracture risk.
- Romosozumab: Boosts bone formation and reduces resorption, effective for high-risk patients.
- Lifestyle Changes:
- Diet: 1,000-1,200 mg calcium and 800-1,000 IU vitamin D daily.
- Exercise: Weight-bearing (e.g., walking) and resistance exercises to strengthen bones.
- Smoking Cessation and Moderation: Avoiding smoking and limiting alcohol to support bone health.
- Fall Prevention: Home safety modifications (e.g., removing rugs), balance training, or assistive devices like canes.
3. Monitoring and Follow-Up
- Regular DEXA scans (every 1-2 years) to track BMD changes.
- Blood tests to monitor calcium, vitamin D, and treatment side effects.
- Ongoing fracture risk assessment using tools like FRAX.
Living with Osteoporosis and Insufficiency Fractures
Insufficiency fractures can be painful and limiting, but with proper treatment, many patients regain function. Keep a record of symptoms, fractures, or falls, and share details with your healthcare team to guide management. Support groups, through organizations like the National Osteoporosis Foundation (nof.org) or online platforms like Reddit, offer a space to connect with others and share coping strategies.
Emotional support is crucial, as fractures and fear of falling can lead to anxiety or reduced activity. Lean on counselors, family, or friends for encouragement. Practical steps, like using supportive footwear, installing grab bars, or practicing balance exercises, can reduce fracture risk and improve confidence.
Why Awareness Matters
Osteoporosis affects over 200 million people worldwide, and insufficiency fractures are a leading cause of disability, yet many cases go undiagnosed until a fracture occurs, per a 2020 review in Osteoporosis International. Raising awareness about the risk of insufficiency fractures and the importance of early osteoporosis diagnosis can prevent life-altering complications.
If you’re over 65, have risk factors (e.g., menopause, steroid use), or experience unexplained back or hip pain, consult a spine specialist, primary care doctor, endocrinologist, or rheumatologist about bone health screening. Resources like the National Osteoporosis Foundation (nof.org) or the International Osteoporosis Foundation (iofbonehealth.org) offer valuable information and support.
By understanding insufficiency fractures and osteoporosis, we can empower individuals to protect their bones and maintain mobility. Let’s keep the conversation going—no one should face the risk of fractures alone.
Disclaimer: This blog post is for informational purposes only and not a substitute for professional medical advice. Consult a healthcare provider for diagnosis and treatment of osteoporosis or insufficiency fractures.



