Interspinous Spacer Devices: A Minimally Invasive Solution for Spinal Canal Stenosis
Lumbar spinal canal stenosis, a condition where the spinal canal in the lower back narrows, can cause significant pain and mobility limitations, particularly through symptoms like spinal claudication—leg pain or weakness triggered by walking or standing. For those who find limited relief from conservative treatments like physical therapy or medications, interspinous spacer devices offer a promising, minimally invasive alternative to traditional surgery.
In this blog post, we’ll explore what lumbar spinal canal stenosis is, how interspinous spacer devices treat it, and what patients can expect, all explained clearly for a general audience.
Understanding Lumbar Spinal Canal Stenosis
Lumbar spinal canal stenosis occurs when the spinal canal in the lower back (lumbar spine, L1-L5) narrows, compressing the spinal cord or nerve roots, particularly the cauda equina. This compression often leads to neurogenic claudication, characterized by leg pain, cramping, numbness, or weakness that worsens with walking or standing and improves with sitting or leaning forward. Common causes include:
- Degenerative Changes: Osteoarthritis, bone spurs, or thickened ligaments (e.g., ligamentum flavum) due to aging.
- Herniated Discs: Bulging discs protruding into the spinal canal.
- Spondylolisthesis: A vertebra slipping forward, further narrowing the canal.
- Congenital Factors: A naturally narrow spinal canal present from birth.
- Other Causes: Trauma, tumors, or conditions like Paget’s disease.
Symptoms typically include centralized low back pain and leg discomfort that limits walking distance, often forcing patients to stop and rest. Lumbar spinal stenosis affects 8-11% of adults over 50, with neurogenic claudication impacting 60-70% of severe cases, per a 2020 study in The Spine Journal.
What Are Interspinous Spacer Devices?
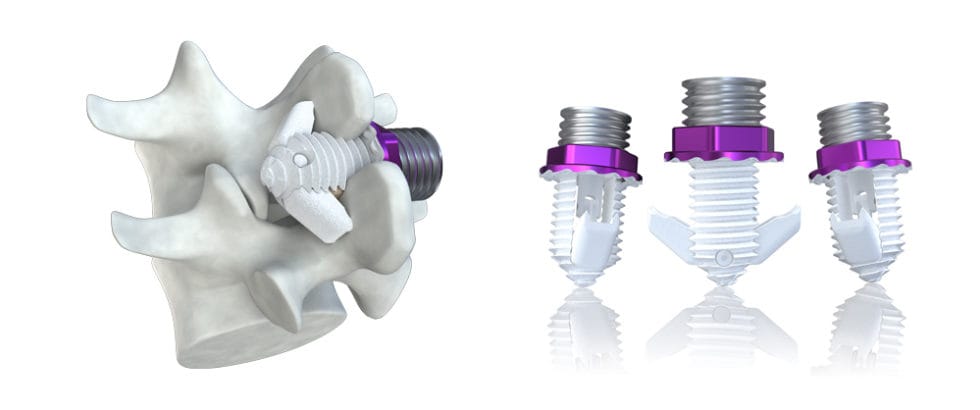
Interspinous spacer devices are small implants placed between the spinous processes—the bony protrusions you can feel along your spine—to relieve nerve compression in lumbar spinal stenosis. These devices work by keeping the vertebrae slightly separated, opening the spinal canal and reducing pressure on nerves. Unlike spinal fusion, which permanently joins vertebrae, spacers preserve spinal motion and are less invasive than traditional surgeries like laminectomy.
The procedure is performed under local anesthesia or mild sedation using imaging guidance (e.g., fluoroscopy). Common devices include the X-Stop, Superion, or Spinal Simplicity, each designed to stabilize the spine while relieving symptoms.
The procedure typically takes 30-60 minutes and is done outpatient.
How Interspinous Spacers Treat Spinal Canal Stenosis
Interspinous spacers address the nerve compression that causes spinal claudication by:
- Opening the Spinal Canal: The device holds the vertebrae apart, increasing space for the spinal cord or nerve roots, particularly during extension (standing or walking).
- Relieving Neurogenic Claudication: By reducing nerve pressure, spacers alleviate leg pain, cramping, or weakness, allowing longer walking distances.
- Preserving Motion: Unlike fusion, spacers maintain some spinal flexibility, reducing stress on adjacent segments.
- Minimizing Tissue Disruption: The procedure avoids extensive muscle or bone removal, leading to faster recovery than open surgery.
Spacers are ideal for patients with:
- Moderate to severe lumbar spinal stenosis (L1-L5) causing neurogenic claudication.
- MRI-confirmed narrowing, often due to thickened ligaments or mild spondylolisthesis.
- Symptoms relieved by sitting or leaning forward (flexion).
- Failed conservative treatments (e.g., physical therapy, epidural injections) but not requiring extensive surgery.
What Does the Evidence Say?
Research supports interspinous spacer devices as an effective, low-risk option for lumbar spinal stenosis with neurogenic claudication. Key findings include:
- Pain and Symptom Relief: A 2020 study in Journal of Neurosurgery: Spine found that 65-75% of patients with spacers reported at least 50% reduction in leg pain and improved walking ability at 6 months.
- Improved Function: A 2019 study in Spine showed that 70% of patients had significant functional improvements (measured by the Oswestry Disability Index), with many walking twice as far without pain at 1 year.
- Long-Term Outcomes: A 2021 review in Pain Physician noted that 60% of patients maintained pain relief and functional gains at 2-5 years, though some required additional treatments if degeneration progressed.
- Safety Profile: A 2020 study in Global Spine Journal reported a low complication rate (<5%), with minimal risks of infection, device migration, or spinous process fracture compared to open surgery.
- Patient Experiences: On platforms like Reddit, patients describe spacers as “a huge relief,” with many regaining mobility for daily activities, though some note mild residual stiffness or the need for physical therapy.
Spacers are not a cure for spinal stenosis, as degenerative changes may continue, and they’re less effective for severe instability, significant spondylolisthesis, or non-claudication pain (e.g., facet joint pain).
What to Expect from Interspinous Spacer Implantation
Here’s an overview of the process:
- Pre-Procedure: Your doctor will review your pain history, symptoms, and MRI to confirm lumbar spinal stenosis and suitability for a spacer. Key indicators include neurogenic claudication and MRI evidence of canal narrowing (e.g., thickened ligamentum flavum). You may need to stop blood thinners or NSAIDs temporarily.
- Procedure: Under local anesthesia or mild sedation, a small incision (1-2 cm) is made in the lower back. Using fluoroscopy, the surgeon places the spacer between the spinous processes of the affected vertebrae (e.g., L4-L5). The procedure takes 30-60 minutes.
- Recovery: Most patients go home the same day. Mild soreness or stiffness at the incision site is common for 1-2 weeks. Light activity can resume within days, with strenuous activity avoided for 4-6 weeks. Pain relief often begins within 1-2 weeks but may take 4-8 weeks to peak.
- Follow-Up: Regular check-ups assess pain relief, mobility, and device stability via X-rays. If symptoms recur due to progressive degeneration, additional treatments (e.g., surgery) may be considered.
- Side Effects: Common side effects include temporary soreness or bruising. Rare risks (<5%) include infection, device migration, spinous process fracture, or nerve irritation, minimized by experienced providers and imaging guidance.
Benefits and Considerations
Benefits:
- Significant relief from leg pain and claudication, often 50-75% reduction.
- Improved walking distance and daily function, enhancing quality of life.
- Minimally invasive with a small incision, low complication rate, and quick recovery.
- Preserves spinal motion, avoiding the rigidity of fusion surgery.
- Outpatient procedure with minimal downtime compared to laminectomy.
Considerations:
- Temporary side effects like soreness or stiffness at the implant site.
- Rare risks include device displacement, infection, or spinous process fracture (<5%).
- Costs range from $10,000-$20,000, with insurance coverage varying (often approved with MRI evidence of stenosis and failed conservative treatments).
- Not suitable for severe spinal instability, significant spondylolisthesis, or non-claudication pain (e.g., disc herniation or facet joint issues).
- Pain may recur if degeneration progresses, requiring further intervention.
Is an Interspinous Spacer Right for You?
Interspinous spacers are typically considered for patients with:
- Moderate to severe lumbar spinal stenosis (L1-L5) causing neurogenic claudication.
- MRI-confirmed canal narrowing, often with thickened ligamentum flavum.
- Symptoms relieved by sitting or leaning forward but not controlled by conservative treatments.
- No significant spinal instability or severe deformity requiring fusion.
Your healthcare team, including a spine surgeon, pain specialist, or interventional radiologist, will assess:
- The source of your pain, using MRI, clinical exams, or diagnostic injections.
- Your overall health, including any contraindications like active infections or bleeding disorders.
- Your goals, such as improved mobility, pain relief, or avoiding open surgery.
Discuss the procedure’s risks, benefits, and expected outcomes with your provider. Choosing a center experienced in interspinous spacers is crucial for safety and success.
Complementary Treatments
Interspinous spacers are often part of a broader pain management plan, including:
- Physical Therapy: Core strengthening, flexion-based exercises, and posture training to support spinal health and enhance recovery.
- Medications: NSAIDs, muscle relaxants, or neuropathic drugs (e.g., gabapentin) for residual pain.
- Interventional Procedures: Epidural steroid injections or spinal cord stimulation for persistent symptoms.
- Lifestyle Changes: Weight management, ergonomic adjustments, and avoiding prolonged standing to reduce spinal stress.
- Psychological Support: Counseling or mindfulness to manage chronic pain’s emotional toll.
A 2021 study in Journal of Neurosurgery: Spine found that combining spacers with physical therapy improved outcomes by 30-40% in stenosis patients, emphasizing a multidisciplinary approach.
Living with Lumbar Spinal Stenosis
Spinal claudication from lumbar stenosis can make walking or standing feel like a chore, but treatments like interspinous spacers offer hope for relief. Keep a symptom diary to track pain triggers and share details with your healthcare team to guide treatment. Support groups, through organizations like Spine-Health (spine-health.com) or the North American Spine Society (spine.org), or online platforms like Reddit, provide a space to connect with others and share coping strategies.
Emotional support is vital, as chronic pain can lead to frustration or depression. Lean on counselors, family, or friends for encouragement. Practical steps, like using a cane, sitting frequently, or practicing flexion-based stretches, can help manage symptoms.
Why Awareness Matters
Lumbar spinal stenosis affects 8-11% of adults over 50, with neurogenic claudication causing significant disability, per a 2020 study in Osteoarthritis and Cartilage. Interspinous spacers are a relatively new option, and many patients are unaware of this less invasive alternative to open surgery. Raising awareness ensures timely diagnosis and access to effective treatments, improving mobility and quality of life.
If you’re struggling with leg pain or limited mobility from lumbar spinal stenosis, talk to a spine specialist, pain management doctor, or interventional radiologist about whether an interspinous spacer could help. Resources like Spine-Health or the American Academy of Orthopaedic Surgeons (aaos.org) offer valuable information and support.
By spotlighting treatments like interspinous spacer devices, we can bring hope and relief to those facing spinal claudication. Let’s keep the conversation going—no one should endure this pain alone.
Disclaimer: This blog post is for informational purposes only and not a substitute for professional medical advice. Consult a healthcare provider before considering interspinous spacer devices or any new treatment for lumbar spinal canal stenosis.



