Sympathetic Nerve Blocks for CRPS: A Path to Pain Relief
Complex Regional Pain Syndrome (CRPS) is a challenging condition marked by intense, chronic pain that can make even the lightest touch unbearable. For those living with CRPS, finding effective treatments is a top priority, and sympathetic nerve blocks have emerged as a promising option.
These procedures target the overactive nervous system at the heart of CRPS, offering potential relief for some patients. In this blog post, we’ll explore what sympathetic nerve blocks are, how they work for CRPS, and what you need to know about this treatment, all explained clearly for a general audience.
What Are Sympathetic Nerve Blocks?
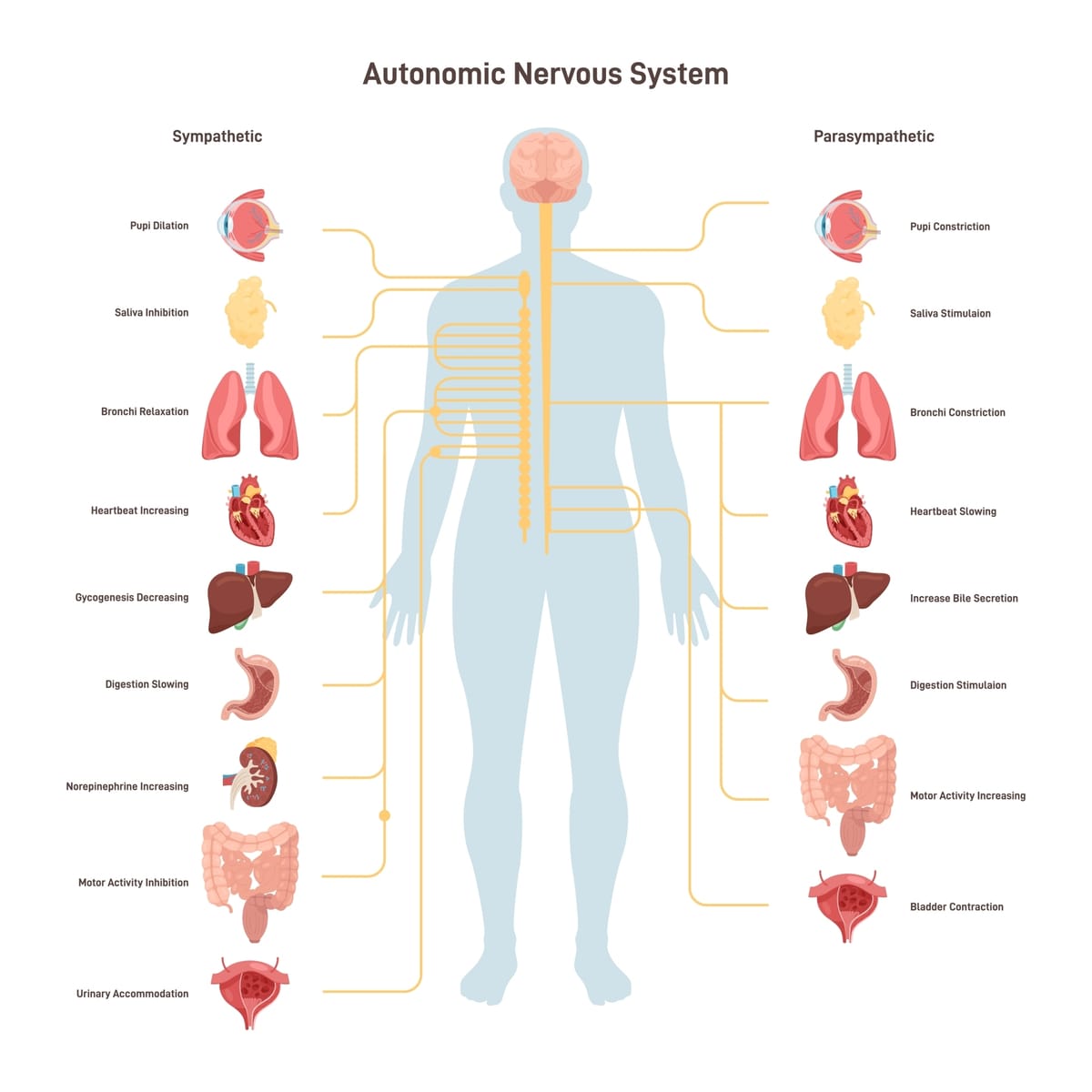
Sympathetic nerve blocks are minimally invasive procedures that involve injecting a local anesthetic (sometimes with a steroid) near specific nerves in the sympathetic nervous system. This system, which controls automatic functions like heart rate and the “fight or flight” response, often becomes overactive in CRPS, amplifying pain and other symptoms. By temporarily “blocking” these nerves, the procedure aims to interrupt the pain cycle and calm the nervous system.For CRPS, two types of sympathetic nerve blocks are commonly used, depending on the affected area:
- Stellate Ganglion Block (SGB): Targets nerves in the neck for CRPS in the arms, hands, or upper body.
- Lumbar Sympathetic Block: Targets nerves in the lower back for CRPS in the legs or feet.
The procedure is typically performed by a specialist using imaging guidance (like ultrasound or X-ray) to ensure accuracy. It takes about 15-30 minutes, and patients can often go home the same day.
Why Use Sympathetic Nerve Blocks for CRPS?
CRPS is driven by a mix of inflammation, nerve dysfunction, and an overactive sympathetic nervous system, which can cause severe pain, swelling, and skin changes. Sympathetic nerve blocks are particularly helpful for CRPS because they:
- Target Pain at the Source: By calming the sympathetic nerves, blocks can reduce the exaggerated pain signals that define CRPS.
- Break the Pain Cycle: Interrupting the feedback loop between nerves and the brain may provide lasting relief, even after the anesthetic wears off.
- Aid Diagnosis: A positive response to a block (e.g., reduced pain or improved symptoms) can confirm that the sympathetic nervous system is involved, helping guide treatment.
Sympathetic nerve blocks are most effective in the early stages of CRPS (within the first 6-12 months) and for “sympathetically maintained pain,” where the sympathetic nervous system plays a key role. However, they can also benefit some patients with longstanding CRPS.
What Does the Evidence Say?
Research on sympathetic nerve blocks for CRPS shows mixed but promising results, with many patients experiencing significant relief. Here’s a look at the current landscape:
- Clinical Studies: A 2016 review in Pain Practice found that sympathetic nerve blocks provided pain relief in 60-80% of CRPS patients, particularly those with early-stage CRPS-I. Stellate ganglion blocks and lumbar sympathetic blocks were both effective, with some patients reporting relief lasting weeks or months.
- Mechanistic Support: Blocks work by reducing sympathetic overactivity, which can lower pain signals and inflammation. They may also improve blood flow to the affected limb, reducing swelling and temperature changes.
- Real-World Insights: Online communities, like Reddit’s CRPS forums, share stories of patients experiencing reduced burning pain or improved mobility after blocks. One user described a stellate ganglion block as “life-changing” for their arm pain, though results vary widely.
- Limitations: Not all CRPS cases are sympathetically driven, so blocks don’t work for everyone. A 2020 study noted that 20-40% of patients may not respond, especially those with CRPS-II or long-term symptoms. Repeat blocks may be needed, and relief isn’t always permanent.
While sympathetic nerve blocks are a standard part of CRPS treatment guidelines (e.g., from the International Association for the Study of Pain), more large-scale studies are needed to optimize their use and predict who will benefit most.
What to Expect from a Sympathetic Nerve Block
If you’re considering a sympathetic nerve block for CRPS, here’s what the process typically involves:
- Procedure: You’ll lie on a table, and the doctor will use imaging to locate the target nerves. After numbing the skin, they’ll inject the anesthetic (and possibly a steroid). You might feel brief discomfort or a warm sensation during the injection.
- Side Effects: Temporary effects depend on the block type. For stellate ganglion blocks, you may experience a droopy eyelid, hoarse voice, or nasal stuffiness (Horner’s syndrome), which resolve within hours. Lumbar blocks may cause leg warmth or mild soreness. Serious complications, like infection or nerve injury, are rare with experienced providers.
- Recovery: Most people go home within a few hours and can resume normal activities the next day. Pain relief, if it occurs, may start within minutes or take a few days.
- Frequency: Some patients benefit from a single block, while others need a series (e.g., weekly for 3-6 weeks) for sustained relief. Your doctor will monitor your response to tailor the plan.
Benefits and ConsiderationsPotential Benefits:
- Significant reduction in pain, swelling, and sensitivity.
- Improved mobility and function in the affected limb.
- May enhance the effectiveness of physical therapy by making movement less painful.
- Minimally invasive with a quick recovery time.
Considerations:
- Temporary side effects like Horner’s syndrome or localized soreness.
- Variable response—not all patients benefit, and relief may fade over time.
- Cost and access—insurance may not always cover blocks for CRPS, and finding a skilled provider can be challenging.
- Not a cure—blocks are most effective when combined with therapies like physical therapy or medications.
Is a Sympathetic Nerve Block Right for You?
Sympathetic nerve blocks are not a first-line treatment for CRPS. Doctors typically recommend starting with conservative measures like physical therapy, medications (e.g., gabapentin or NSAIDs), and lifestyle changes. If these don’t provide enough relief, or if your CRPS symptoms suggest sympathetic involvement (e.g., burning pain, swelling, or temperature changes), a nerve block could be a next step.
Before pursuing a block, consider:
- Consulting a pain specialist or neurologist familiar with CRPS to confirm your diagnosis and assess if your pain is sympathetically maintained.
- Discussing the procedure’s risks, benefits, and expected outcomes with your doctor.
- Checking insurance coverage, as costs for non-covered blocks can add up.
The Road AheadSympathetic nerve blocks offer hope for many living with CRPS, providing a targeted way to ease debilitating pain and reclaim some quality of life. While they’re not a universal fix, their role in breaking the pain cycle makes them a valuable tool, especially when used early and alongside other treatments. Ongoing research, including trials listed on Clinicaltrials.gov, aims to refine their use and explore combinations with therapies like spinal cord stimulation.
If you’re navigating CRPS, talk to your healthcare team about whether sympathetic nerve blocks could be part of your plan. Connecting with CRPS communities, like those through the Reflex Sympathetic Dystrophy Syndrome Association (rsds.org) or online forums, can also offer support and insights from others who’ve tried this approach.
CRPS is a tough road, but treatments like sympathetic nerve blocks show that relief is possible. Keep advocating for yourself, and don’t lose hope—you’re not alone in this fight.
Disclaimer: This blog post is for informational purposes only and not a substitute for professional medical advice. Consult a healthcare provider before considering sympathetic nerve blocks or any new treatment for CRPS.



