Understanding Complex Regional Pain Syndrome (CRPS)
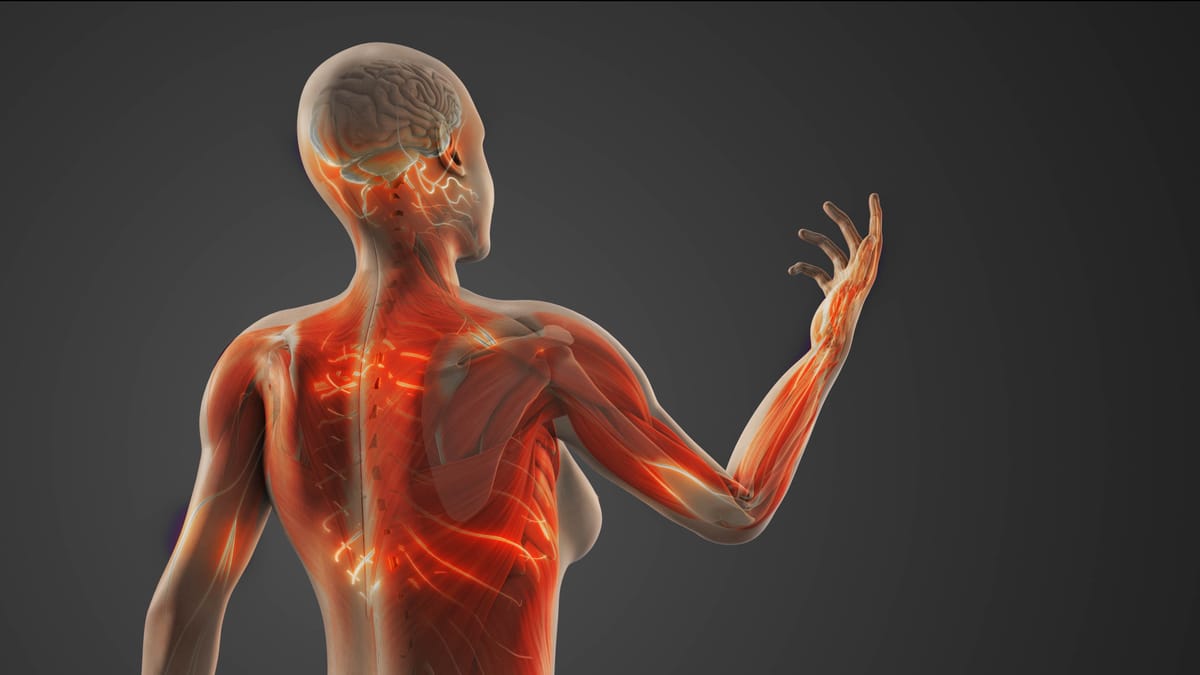
Complex Regional Pain Syndrome (CRPS) is a condition that can turn everyday sensations into overwhelming pain, often leaving those affected feeling frustrated and misunderstood.
Though it’s relatively rare, CRPS can profoundly impact quality of life, and awareness is key to supporting those who live with it. In this blog post, we’ll break down what CRPS is, its symptoms, causes, and treatment options in a way that’s clear and accessible for everyone.
What is CRPS?
CRPS is a chronic pain condition characterized by intense, prolonged pain that’s disproportionate to the initial injury or trigger. It typically affects one limb—such as an arm, leg, hand, or foot—but can spread to other areas. The pain is driven by a malfunction in the nervous system, where the brain and nerves misfire, amplifying pain signals and causing other symptoms like swelling or skin changes.
There are two types of CRPS:
- CRPS-I: Occurs without confirmed nerve damage, often after a minor injury like a sprain or fracture.
- CRPS-II: Involves confirmed nerve damage, typically following a more significant injury, like a crush or surgical trauma.
CRPS is estimated to affect 200,000 people annually in the U.S., with women being three to four times more likely to develop it than men. It can occur at any age but is most common in adults aged 40-60.
What Are the Symptoms?
CRPS symptoms can vary widely and often seem out of proportion to the original injury. They typically include:
- Severe, Persistent Pain: Described as burning, throbbing, or stabbing, often in one limb. The pain may feel constant or flare with touch or movement.
- Sensitivity to Touch or Temperature: Even light contact, like clothing brushing the skin, can be excruciating (a condition called allodynia). Cold or heat may also trigger pain.
- Swelling and Skin Changes: The affected area may swell, feel warm or cool, or show changes in color (red, blue, or mottled) or texture (shiny or thin skin).
- Stiffness and Mobility Issues: Joints may become stiff, and muscles may weaken, making movement difficult.
- Abnormal Hair or Nail Growth: Hair may grow faster or slower, and nails may become brittle or grooved.
- Tremors or Muscle Spasms: Involuntary movements or muscle contractions can occur.
Symptoms may change over time, sometimes spreading to other parts of the body. Early diagnosis is critical, as CRPS can worsen without intervention.
What Causes CRPS?
The exact cause of CRPS isn’t fully understood, but it’s thought to involve a combination of nerve dysfunction, inflammation, and changes in how the brain processes pain. Common triggers include:
- Injuries: Fractures, sprains, burns, or even minor trauma can spark CRPS, especially in CRPS-I.
- Nerve Damage: Direct nerve injuries, like those from surgery or accidents, often lead to CRPS-II.
- Surgery: Post-surgical inflammation or nerve irritation can trigger CRPS.
- Other Factors: In rare cases, CRPS develops without a clear injury, possibly linked to infections, strokes, or autoimmune conditions.
Risk factors include a history of intense pain responses, autoimmune disorders, or psychological stress, though stress alone doesn’t cause CRPS. The condition likely results from a “perfect storm” of genetic, neurological, and environmental factors.
How is CRPS Diagnosed?
Diagnosing CRPS can be challenging because there’s no single test for it, and symptoms overlap with other conditions like arthritis or neuropathy. Doctors rely on:
- Medical History and Symptom Review: Detailing the injury and symptoms helps identify CRPS patterns.
- Physical Exam: Checking for pain, swelling, skin changes, or temperature differences in the affected area.
- Budapest Criteria: A widely used guideline that lists specific signs and symptoms, like allodynia, swelling, and asymmetry, to confirm CRPS.
- Tests to Rule Out Other Conditions: Imaging (X-rays, MRIs) or nerve studies may be used to exclude other causes.
Early diagnosis—ideally within the first few months—is crucial to prevent progression, so seeing a pain specialist or neurologist familiar with CRPS is key.
Managing and Treating CRPS
There’s no cure for CRPS, but a combination of treatments can reduce pain, improve function, and enhance quality of life. The goal is to calm the nervous system, manage symptoms, and prevent worsening. Common approaches include:
- Medications:
- Pain relievers (e.g., NSAIDs or opioids for severe cases).
- Antidepressants or anticonvulsants (e.g., gabapentin) to address nerve pain.
- Corticosteroids or bisphosphonates to reduce inflammation or bone changes.
- Physical and Occupational Therapy:
- Gentle exercises to maintain mobility and strength.
- Desensitization techniques to reduce sensitivity to touch.
- Mirror therapy, where a mirror helps “retrain” the brain to reduce pain perception.
- Interventional Procedures:
- Sympathetic Nerve Blocks: Injections, like stellate ganglion blocks, to calm overactive nerves.
- Spinal Cord Stimulation: A device implanted to disrupt pain signals.
- Ketamine Infusions: Low-dose ketamine may help reset pain pathways in severe cases.
- Psychological Support:
- Cognitive Behavioral Therapy (CBT) to cope with chronic pain and stress.
- Support groups to connect with others living with CRPS.
- Lifestyle Changes:
- Stress management techniques like mindfulness or meditation.
- A balanced diet and adequate sleep to support overall health.
Treatment is highly individualized, and what works for one person may not work for another. A multidisciplinary team—including pain specialists, physical therapists, and mental health professionals—often yields the best results.
Living with CRPS: A Personal Perspective
CRPS can feel like an invisible illness. The pain is real, but others may not see or understand it, leading to frustration or isolation. Simple tasks, like holding a cup or walking, can become monumental challenges. Yet, many people with CRPS find ways to adapt, whether through pacing activities, using assistive devices, or leaning on supportive communities.
Self-advocacy is crucial. Keeping a symptom journal, seeking out CRPS-savvy doctors, and connecting with organizations like the Reflex Sympathetic Dystrophy Syndrome Association (rsds.org) can empower you. It’s also okay to grieve the changes CRPS brings while celebrating small victories, like a low-pain day or mastering a new coping strategy.
Why Awareness Matters
CRPS is often misdiagnosed or dismissed, which delays treatment and worsens outcomes. Raising awareness helps ensure faster diagnoses, better care, and more empathy for those affected. If you or someone you know has persistent, unexplained pain after an injury, don’t hesitate to ask about CRPS.
By sharing knowledge, we can build a world where CRPS is better understood and those living with it feel supported. Let’s keep the conversation going—no one should face CRPS alone.
Disclaimer: This blog post is for informational purposes only and not a substitute for professional medical advice. Always consult a healthcare provider for diagnosis and treatment.



