Understanding Pain After Spine Surgery: Causes and Insights for Recovery
Spine surgery is often used to treat conditions like herniated discs, spinal stenosis, or scoliosis. However, some patients experience persistent or new pain after surgery, which can be frustrating and concerning. Known as post-surgical spine pain or "failed back surgery syndrome" (FBSS) in some cases, this pain can stem from various sources.
In this blog post, we’ll explore the common causes of pain after spine surgery, how they manifest, and what you can do
Why Pain Persists or Develops After Spine Surgery
Pain after spine surgery can arise from the surgical procedure itself, pre-existing conditions, or new issues that develop during recovery. While many patients experience significant relief after surgery, 10-40% report ongoing or new pain, per a 2019 study in The Spine Journal. This doesn’t necessarily mean the surgery “failed”—pain can have multiple causes, and understanding them is key to finding relief. Below, we’ll break down the primary sources of post-surgical spine pain.
Common Causes of Pain After Spine Surgery
1. Surgical Site Pain
- What It Is: Pain at the incision site or surrounding tissues due to the surgery itself.
- Why It Happens: Cutting through skin, muscles, and other tissues causes inflammation and trauma. Even minimally invasive procedures can irritate tissues, leading to temporary pain.
- Symptoms: Localized soreness, tenderness, or aching at the incision site, often worse with movement or pressure.
- Prevalence: Common in the first 2-8 weeks post-surgery, typically improving with healing, per a 2020 review in Journal of Orthopaedic Surgery and Research.
- Example: Pain after a lumbar fusion may feel like muscle soreness around the lower back incision.
2. Residual or Recurrent Disc Issues
- What It Is: Pain from incomplete resolution or recurrence of disc-related problems.
- Why It Happens:
- Incomplete Decompression: In procedures like discectomy, some disc material or bone spurs may remain, continuing to press on nerves.
- Recurrent Herniation: A new disc herniation can occur at the same or adjacent level, often within months of surgery.
- Symptoms: Radiating pain, numbness, or tingling in the legs or arms (sciatica or radiculopathy), similar to pre-surgical symptoms.
- Prevalence: Recurrent herniation occurs in 5-15% of discectomy patients, per a 2018 study in Spine.
3. Nerve Irritation or Damage
- What It Is: Pain from nerves affected during surgery or pre-existing nerve damage that persists.
- Why It Happens:
- Surgical Manipulation: Nerves may be irritated during surgery from retraction or handling.
- Scar Tissue (Epidural Fibrosis): Scar tissue can form around nerves, causing compression or tethering.
- Neuropathic Pain: Pre-existing nerve damage (e.g., from chronic compression) may not fully resolve post-surgery.
- Symptoms: Burning, shooting, or electric-shock-like pain, often radiating to the limbs, with possible numbness or weakness.
- Prevalence: Neuropathic pain affects 20-30% of spine surgery patients, per a 2021 study in Pain Medicine.
4. Adjacent Segment Disease (ASD)
- What It Is: Pain from degeneration in spinal segments above or below the surgical site.
- Why It Happens: Fusion surgeries (e.g., spinal fusion) alter spinal mechanics, placing extra stress on adjacent discs or joints, leading to accelerated wear, disc herniation, or arthritis.
- Symptoms: New or worsening back or neck pain, sometimes with radiating symptoms, appearing months to years after surgery.
- Prevalence: ASD occurs in 10-30% of fusion patients within 5-10 years, per a 2019 study in Journal of Neurosurgery: Spine.
5. Facet Joint Pain
- What It Is: Pain from the small stabilizing joints (facet joints) in the spine.
- Why It Happens:
- Surgical Stress: Fusion or decompression can overload facet joints, causing inflammation or arthritis.
- Pre-existing Degeneration: Facet joint issues may persist or worsen post-surgery.
- Symptoms: Localized back or neck pain, worse with twisting, bending, or prolonged sitting/standing.
- Prevalence: Facet joint pain contributes to 15-25% of post-surgical pain cases, per a 2020 review in Global Spine Journal.
6. Muscle Spasms or Myofascial Pain
- What It Is: Pain from muscles or connective tissues around the spine.
- Why It Happens:
- Surgical Trauma: Muscle dissection during surgery can cause spasms or tightness.
- Postural Changes: Altered spinal mechanics or prolonged immobility during recovery can strain muscles.
- Symptoms: Tightness, cramping, or aching in the back or neck, often relieved by stretching or heat.
- Prevalence: Muscle-related pain is common in the early recovery phase, affecting 30-40% of patients, per a 2018 study in Orthopedics.
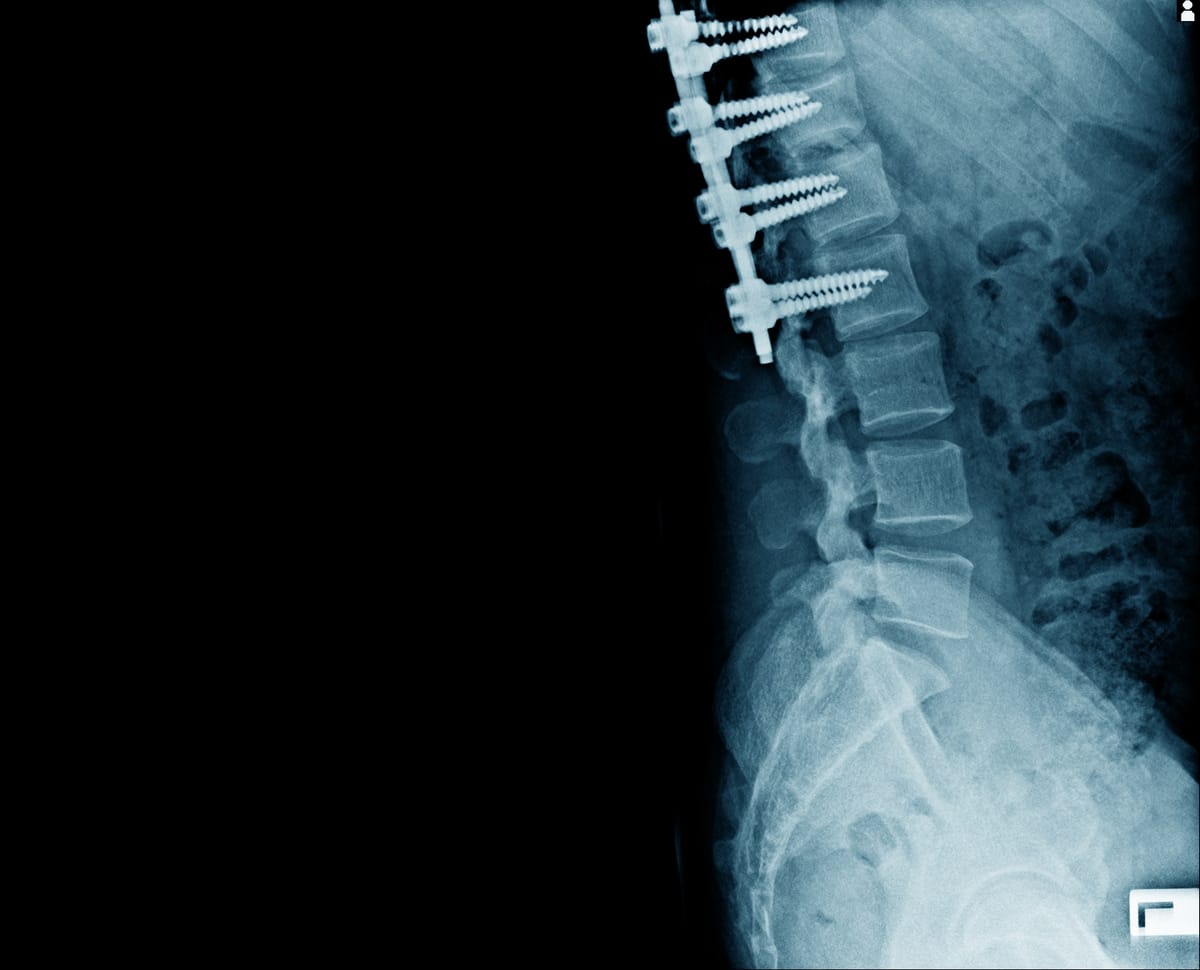
7. Hardware-Related Pain
- What It Is: Pain from surgical implants like screws, rods, or plates used in spinal fusion.
- Why It Happens:
- Implant Irritation: Hardware may irritate surrounding tissues or nerves.
- Loosening or Failure: Implants can loosen or break, causing instability or pain.
- Infection: Rare infections around hardware can cause localized pain.
- Symptoms: Deep, aching pain at the surgical site, sometimes with swelling or warmth if infection is present.
- Prevalence: Hardware issues contribute to pain in 5-10% of fusion patients, per a 2019 study in Spine.
8. Infection or Inflammation
- What It Is: Pain from post-surgical infections or excessive inflammation.
- Why It Happens:
- Surgical Site Infection: Bacteria can infect the incision or deeper tissues, including hardware.
- Inflammatory Response: Excessive inflammation post-surgery can irritate tissues or nerves.
- Symptoms: Redness, swelling, warmth, or fever, along with persistent pain, sometimes with drainage.
- Prevalence: Infections occur in 1-5% of spine surgeries, per a 2020 study in Journal of Orthopaedic Surgery.
9. Failed Back Surgery Syndrome (FBSS)
- What It Is: A catch-all term for persistent or new pain after spine surgery, encompassing multiple causes.
- Why It Happens: Factors include incomplete decompression, recurrent pathology, scar tissue, or unrealistic expectations about surgical outcomes.
- Symptoms: Ongoing or new back, neck, or radiating pain, often similar to or worse than pre-surgical symptoms.
- Prevalence: FBSS affects 10-40% of spine surgery patients, per a 2019 study in The Spine Journal.
10. Psychological and Referred Pain
- What It Is: Pain influenced by emotional factors or originating from non-spinal sources.
- Why It Happens:
- Psychological Amplification: Anxiety, depression, or stress can heighten pain perception, common post-surgery due to recovery challenges.
- Referred Pain: Pain from other areas (e.g., hip or pelvic issues) may be felt in the back.
- Symptoms: Diffuse, aching pain that may not align with surgical findings, often with emotional distress.
- Prevalence: Psychological factors contribute to 20-30% of post-surgical pain cases, per a 2018 study in Psycho-Oncology.
Managing Post-Surgical Spine Pain
Addressing pain after spine surgery requires identifying its cause through a thorough evaluation, including physical exams, imaging (e.g., X-rays, MRI), or diagnostic injections.
Treatment options include:
- Medications: NSAIDs, muscle relaxants, or neuropathic drugs (e.g., gabapentin) for pain and inflammation.
- Physical Therapy: Strengthening core muscles, improving posture, and reducing scar tissue adhesion.
- Interventional Procedures:
- Epidural steroid injections for nerve irritation.
- Facet joint injections or radiofrequency ablation for joint pain.
- Spinal cord stimulation for neuropathic pain.
- Basivertebral Nerve Ablation (BVNA) for pain arising from treated or untreated vertebrae.
- Minimally Invasive Lumbar Decompression(MILD) for new or recurrent spinal canal narrowing.
- Surgical Revision: In cases of hardware failure, infection, or significant recurrent pathology, though rare (5-10% of cases).
- Psychological Support: Cognitive-behavioral therapy or counseling to address emotional factors.
- Lifestyle Changes: Weight management, gentle exercise, and ergonomic adjustments to reduce strain.
A 2021 study in Global Spine Journal found that a multidisciplinary approach, combining physical therapy and targeted interventions, improved outcomes in 60-70% of patients with post-surgical pain.
Living with Post-Surgical Pain
Persistent pain after spine surgery can feel disheartening, but it doesn’t mean recovery is impossible. Keep a pain diary to track symptoms and triggers, and communicate openly with your surgeon or pain specialist. Support groups, through organizations like the Spine Health Foundation or online platforms like Reddit, offer a space to share experiences and coping strategies.
Emotional support is crucial, as chronic pain can amplify stress or depression. Lean on counselors, family, or friends for encouragement. Practical steps, like pacing activities, using heat/ice, or practicing relaxation techniques, can also help.
Why Awareness Matters
Post-surgical spine pain affects a significant number of patients, yet it’s often misunderstood or attributed solely to “failed surgery.” Understanding its diverse causes empowers patients to seek targeted treatments and advocate for their care. Early intervention can prevent chronic pain and improve outcomes.If you’re experiencing pain after spine surgery, don’t hesitate to consult a pain specialist, or neuro-interventionalist.
By shedding light on the causes of post-surgical spine pain, we can help patients navigate their recovery with hope and clarity. Let’s keep the conversation going—no one should face this pain alone.
Disclaimer: This blog post is for informational purposes only and not a substitute for professional medical advice. Consult a healthcare provider for diagnosis and treatment of pain after spine surgery.



